4 Signs Your Stress And Gut Health Are Connected (And Ruining Your Sleep)
You’ve noticed it: bloating that gets worse as the day drags on. The 3 a.m. wake-ups where your mind races and won’t shut off. That relentless craving for sugar or carbs around 4 p.m. You chalk it up to a stressful week at work, maybe something you ate, or just “getting older.”
But here’s what most people miss—these aren’t three separate problems. They’re connected. And the thread linking them runs straight through your gut.
The Science: How Stress And Gut Health Are Connected (And How It Ruins Sleep)
Stress triggers your body to release cortisol and adrenaline into your blood. That’s normal. The problem starts when stress becomes chronic. Elevated cortisol levels don’t just make you feel anxious—they actively reshape your gut microbiome (NIH).
What Happens When Stress Becomes Chronic
- Chronic cortisol elevation may affect your gut lining — Chronic stress is associated with changes in gut barrier function, which research suggests may affect how the digestive system processes nutrients and bacteria. (NIH)
- Your gut-brain connection malfunctions — The direct communication highway between your digestive system and brain breaks down
- Inflammation spikes — Triggering both anxiety and gut health problems simultaneously
- Sleep chemicals drop — Your gut bacteria produce less serotonin and GABA (calming brain chemicals that help you sleep) (NIH)
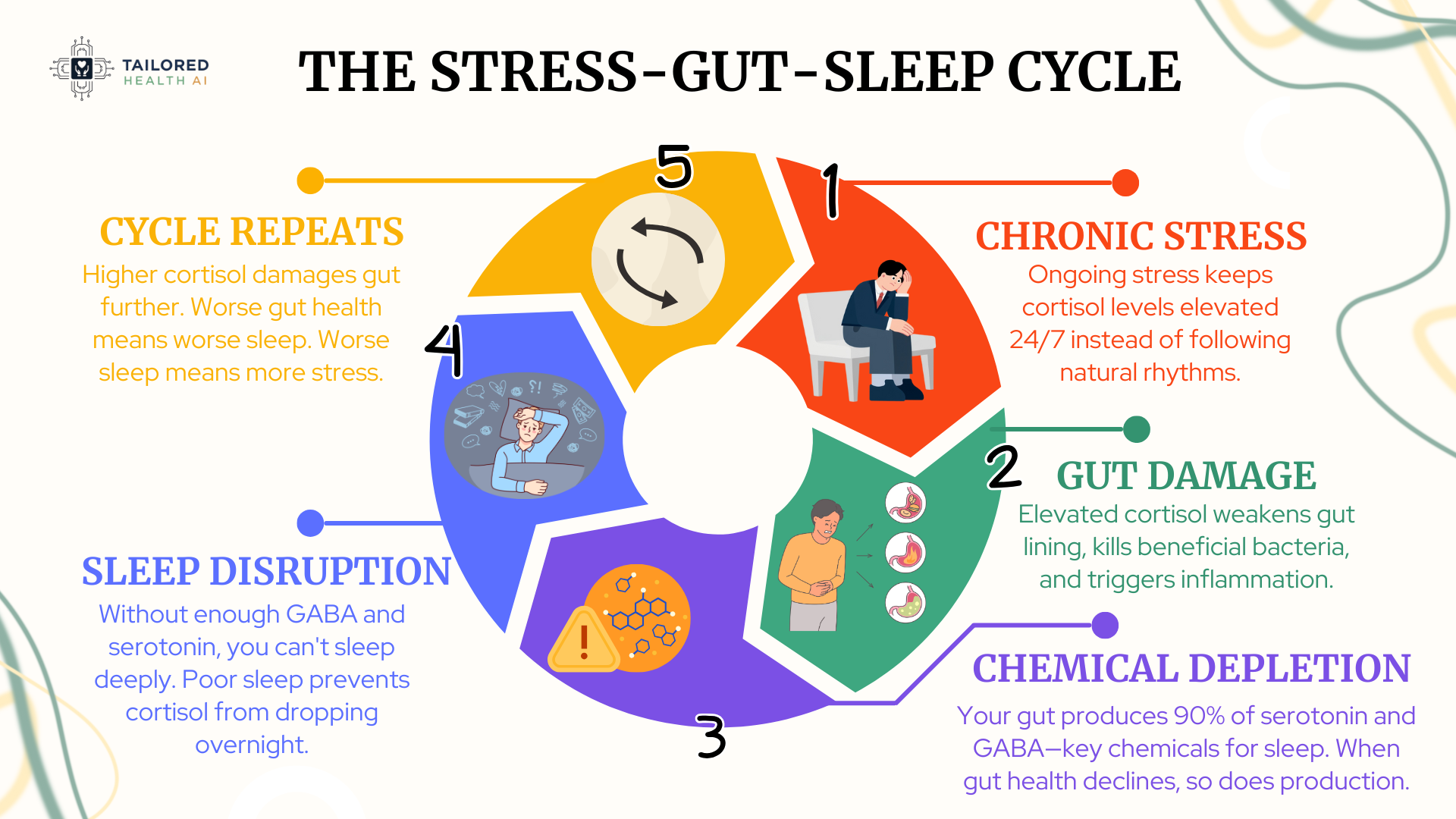
The Vicious Cycle:
| What Happens | The Effect | What Comes Next |
|---|---|---|
| Chronic stress | Damages gut bacteria | Fewer sleep chemicals |
| Poor sleep | Raises cortisol levels | More gut damage |
| Gut inflammation | Increases anxiety | More stress hormones |
This isn’t about willpower or “just relaxing more.” When stress affects gut health at a biological level, you can’t think your way out of digestive issues or insomnia. Here’s what’s really going on inside your digestive system.
The signs are specific. And once you recognize them, you can address the root cause instead of chasing symptoms.
Is Your Stress Ruining Your Sleep Through Your Gut?
Most people spend months trying random supplements and “stress reduction tips” that don’t work because they’re guessing. Your body’s stress response is as unique as your fingerprint.
Sign #1: Your Belly Bloats as the Day Goes On
You start the morning feeling fine. By mid-afternoon, your jeans feel snug. By evening? You’re unbuttoning your pants, wondering why you look six months pregnant. This isn’t about what you ate for dinner—it’s what stress did to your digestion all day long.
Why Your Digestion Declines Throughout the Day
| Time of Day | Digestive Function | Bloating Risk |
|---|---|---|
| Morning | Enzymes peak, motility strong | Low |
| Afternoon | Starting to decline | Medium |
| Evening | Lowest efficiency | High |
The Stress and Gut Health Connection Explained
- Cortisol slows digestion — Food sits in your gut longer and creates more gas (NIH)
- Your body makes fewer enzymes — Your body produces fewer enzymes to break down fats and proteins (NIH)
- Your body’s clock works against you — Your digestion naturally slows down by the time evening arrives (NIH)
- Food moves erratically through your gut — Food sits too long in certain spots of your digestive tract
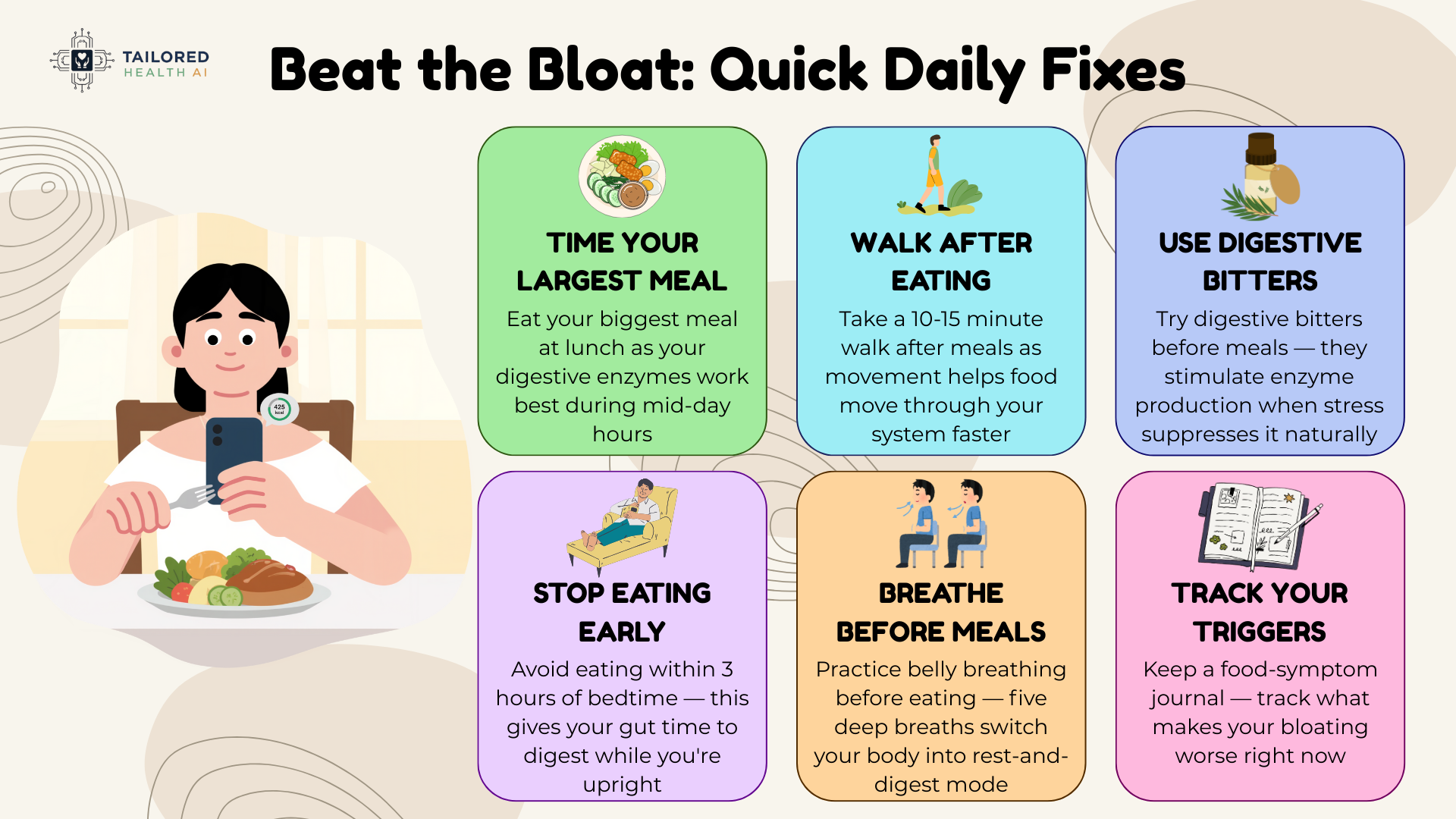
Quick Fixes You Can Try Today
• Eat your largest meal at lunch — Your digestive enzymes work best during mid-day hours
• Take a 10-15 minute walk after meals — Movement helps food move through your system faster
• Try digestive bitters before meals — Bitters stimulate enzyme production when stress suppresses it naturally
• Avoid eating within 3 hours of bedtime — This gives your gut time to digest while you’re upright
• Practice belly breathing before eating — Five deep breaths switch your body into rest-and-digest mode
• Keep a food-symptom journal — Track what makes your bloating worse right now
Sign #2: You’re Wide Awake at 3 AM—Every Night
You wake up at 3 am., heart racing, mind spinning through tomorrow’s to-do list. You try to fall back asleep, but your brain won’t cooperate. This isn’t random insomnia—it’s a cortisol spike hijacking your sleep cycle.
Normal vs. Stressed Cortisol Patterns
| Time | Normal Cortisol | Stressed Cortisol | Result |
|---|---|---|---|
| 3 AM | Low (sleep maintenance) | Spike | Wake up alert, can’t fall back asleep |
| 7 AM | Peak (wake naturally) | Already elevated | Wake feeling unrested |
| Evening | Low (prepare for sleep) | Still high | Difficulty falling asleep |
Why This Happens
- Your stress system stays on — Cortisol spikes at the wrong times instead of following your natural rhythm (Johns Hopkins Medicine)
- The 3 a.m. spike pulls you awake — The cortisol spike disrupts your deep sleep phases and jolts you awake (Sleep Foundation)
- Stress kills sleep-friendly gut bacteria — Your gut makes less GABA and serotonin, the chemicals your brain needs for sleep (NIH)
- Cortisol and gut inflammation feed each other — This creates leaky gut and disrupts your sleep cycle even more (Mayo Clinic)
What You Can Do Tonight
• No screens 1-2 hours before bed — Blue light from screens triggers cortisol release at the wrong time
• Consider magnesium glycinate supplementation — Research suggests magnesium at 200-400mg may support cortisol regulation and GABA production (Check with your doctor if you have kidney issues or take medications)
• Keep a notepad by your bed — Brain dump your racing thoughts to shut down the stress response
• Avoid caffeine after 12 PM — Caffeine’s 6-hour half-life keeps cortisol elevated into the evening
• Practice 4-7-8 breathing if you wake — Breathe in for 4 counts, hold for 7, breathe out for 8
• Consider a small protein snack before bed — Stable blood sugar prevents the cortisol spike that wakes you overnight
Recognizing These Signs in Yourself?
The problem? Generic protocols don’t account for YOUR cortisol pattern or YOUR specific gut imbalances. That’s why most advice helps a little—but doesn’t fix the root cause.
Sign #3: You’re Raiding the Pantry for Sweets and Comfort Food Late at Night
Around 4 p.m., you’d trade your laptop for a cookie. By 8 p.m., you’re standing in front of the pantry, hunting for something sweet. This isn’t a lack of willpower—it’s your stress hormones manipulating your brain’s reward system.
The Stress-Sugar Craving Cycle
| What Happens | Why Sugar Cravings At Night | The Problem |
|---|---|---|
| Cortisol stays elevated all day | Your brain gets desperate for quick energy from glucose | You eat sugar, spike insulin, crash harder |
| Gut bacteria become imbalanced | Damaged microbes send stronger craving signals to your brain | The “bad” bacteria literally demand more sugar to survive |
| Serotonin production drops | Your body uses sugar to temporarily boost feel-good chemicals | You’re self-medicating stress with food |
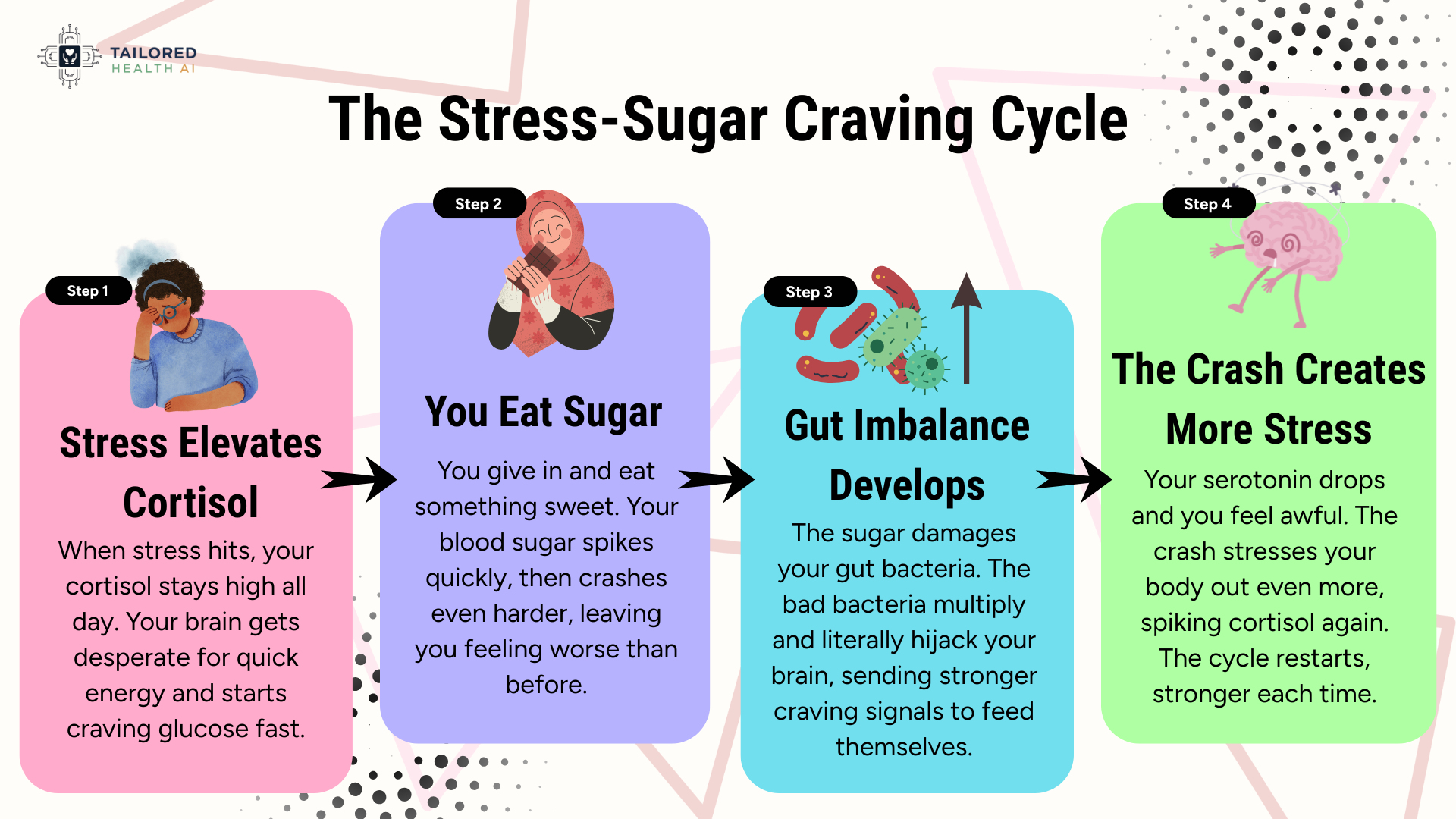
Why This Happens
- High cortisol makes your brain crave fast energy — Chronic stress depletes your glucose reserves, making your brain desperate for quick fuel from sugar (Harvard Health)
- Your gut bacteria actually control your cravings — Stressed gut bacteria produce chemicals that manipulate your eating behavior and increase sugar-seeking (NIH)
- Sugar temporarily calms your stress response — Eating sugar activates the same reward pathways as addictive substances, giving short-term relief from anxiety (NIH)
- Evening cortisol disrupts blood sugar regulation — When cortisol should drop at night, it stays elevated and creates unstable blood sugar that triggers cravings (Cleveland Clinic)
What You Can Do Tonight
• Eat protein with every meal — Protein stabilizes blood sugar for 3-4 hours and reduces evening cravings significantly
• Choose fiber-rich carbs earlier in the day — Oats, quinoa, and sweet potatoes provide steady energy without the sugar crash
• Consider L-theanine supplementation — Research shows L-theanine at 100-200mg may help reduce cortisol and stress-related cravings.
• Keep pre-portioned healthy snacks visible — Nuts, Greek yogurt, or dark chocolate satisfy cravings without feeding the stress cycle
• Take a 5-minute walk when cravings hit — Movement resets your cortisol response and reduces immediate sugar-seeking behavior
• Address your actual stress before 4 p.m. — The craving is a symptom, not the problem itself
Sign #4: When Your Gut Acts Up, Your Mind Won’t Stop Worrying
If you’re dealing with both anxiety and digestive issues, that’s not a coincidence. Your gut and brain are in constant conversation through the gut-brain connection, and when one struggles, it drags the other down with it.
The Two-Way Street: How Gut and Brain Affect Each Other
| Direction | What Happens | The Result |
|---|---|---|
| Brain → Gut | Anxiety triggers stress hormones that damage gut lining and alter bacteria balance | Bloating, cramping, diarrhea, constipation |
| Gut → Brain | Inflamed gut sends distress signals through the vagus nerve (the main nerve connecting your gut and brain) | Racing thoughts, panic sensations, heightened worry |
Why This Happens
- Your gut produces 90% of your body’s serotonin — When gut bacteria are imbalanced from stress, serotonin production drops and anxiety symptoms intensify (Harvard Health)
- The vagus nerve (the main connection between gut and brain) creates a direct highway — Gut inflammation travels straight to your brain as anxiety signals, while brain-based stress travels down as digestive problems (Johns Hopkins Medicine)
- Stress hormones kill beneficial gut bacteria that regulate mood — Cortisol actively reshapes your gut bacteria, reducing the bacteria that produce calming brain chemicals like GABA (NIH)
- An inflamed gut creates a vicious cycle with anxiety — Leaky gut allows bacterial toxins into your bloodstream, triggering immune responses that amplify both anxiety and digestive symptoms (Stanford Medicine)
What You Can Do Starting Now
• Consider probiotics with specific strains — Research on Lactobacillus and Bifidobacterium suggests these may produce mood-regulating brain chemicals. Consult your doctor before starting any supplement.
• Try Vagus nerve stimulation through deep breathing exercises — Slow belly breathing for 5 minutes activates your body’s calming response
• Eliminate inflammatory foods for 2-3 weeks to test gut response — Remove gluten, dairy, and processed sugar to see if gut symptoms and anxiety improve together
• Explore omega-3 supplementation — Research suggests omega-3s at 1000-2000mg daily may help reduce inflammation.
• L-glutamine is an amino acid studied in research on digestive health. Common study doses are around 5g daily. Your provider can help determine if supplementation might be relevant to your wellness goals.
• Track both gut and mood symptoms in a daily journal — You’ll see patterns showing how addressing one problem improves the other automatically
Stop Guessing. Get Personalized Insights Into Your Stress-Gut-Sleep Patterns.
Here’s the truth: Your cortisol rhythm is unique. Your gut bacteria composition is unique. Your sleep architecture is unique. Cookie-cutter protocols fail because they ignore YOUR biology.
FAQs: Your Common Questions Answered Here
⚠️Important Information
This content is for educational and informational purposes only. We’re sharing information, not providing medical advice, diagnosing conditions, or recommending treatments. Individual responses to stress, supplements, and lifestyle changes vary significantly. Always consult a qualified healthcare provider before starting any new supplement regimen or making significant changes to address health concerns. The information provided here should not replace professional medical guidance tailored to your specific situation.
