Burnout vs. Depression: Why Your Doctor Can’t Tell (And What Tests Actually Can)
Introduction: Why Your Doctor Can’t Tell If It’s Depression or Burnout
You’ve been dragging yourself through life for months. Maybe years.
You finally worked up the energy to see your doctor. You described the exhaustion, the brain fog, the fact that getting out of bed feels like climbing Everest.
You expected answers. Tests. Something concrete.
Instead, you got a questionnaire.
Nine questions on a sheet of paper. How often have you felt down, depressed, or hopeless in the last two weeks? Circle a number. Add up your score. If it’s above 10, congratulations—you’re depressed. Here’s a prescription for an SSRI and a recommendation to “reduce stress.”
But here’s the thing: what if you’re not depressed? What if you’re burned out? Or what if you have no idea which one it is because the symptoms look almost identical?
The Problem: Your Doctor Is Guessing
Your doctor isn’t being lazy. They’re following the diagnostic playbook:
How doctors currently diagnose:
- Depression: PHQ-9 questionnaire + clinical interview (APA)
- Burnout: Maslach Burnout Inventory + symptom checklist (ResearchGate)
The issue? Both rely entirely on self-reported symptoms:
- ✅ Fatigue
- ✅ Lost motivation
- ✅ Sleep problems
- ✅ Difficulty concentrating
- ✅ Feeling hopeless or detached
The issue? Both rely entirely on self-reported symptoms:
The issue? Both rely entirely on self-reported symptoms:
- Scenario 1: Burnout treated as depression
- Your body: Elevated cortisol, exhausted adrenals, fight-or-flight stuck on
- Treatment: Antidepressants + therapy
- Result: ❌ Nothing changes (SSRIs won’t fix cortisol dysregulation)
- Scenario 2: Depression treated as burnout
- You quit your job, take a sabbatical, and try adaptogens.
- Result: ❌ Still feel terrible (burnout strategies won’t fix neurotransmitter dysfunction)
The issue? Both rely entirely on self-reported symptoms:
Your Body Holds the Answer
If you’ve Googled “burnout or depression test” or taken a “burnout vs depression quiz,” you know how unsatisfying those results are. More questions. More subjective scoring. No clarity.
What you actually want: Objective answers about what’s happening in your body—not just how you feel.
Here’s what your doctor probably hasn’t told you: Your biology holds clues that questionnaires can’t capture.
Burnout and depression may look similar on paper, but they show up differently in:
- 🩸 Your bloodwork
- 🧬 Your hormone levels
- 🔥 Your inflammatory markers
In this article, we’re covering:
- Burnout vs depression symptoms (side-by-side comparison)
- 5 tests that might differentiate between the two
- FAQ (how to get tested, how to interpret results)
This isn’t about self-diagnosing. It’s about giving you the tools to advocate for better testing and stop wasting time on treatments that were never going to work.
Let’s start with the symptoms.
Struggling to Tell the Difference?
Burnout vs Depression: Symptoms Comparison
Here’s where things get tricky. Burnout and depression share so many overlapping symptoms that even experienced clinicians struggle to tell them apart based on how you feel alone.
But there are subtle differences—especially in context, triggers, and recovery patterns—that can offer clues.
This table breaks down the key differences between burnout and depression symptoms:
| Symptom | Burnout | Depression |
|---|---|---|
| Fatigue | Related to overwork; improves slightly with rest or vacation | Persistent and pervasive; doesn’t improve with rest alone |
| Motivation | Lost interest in work specifically; hobbies may still feel appealing | Lost interest in everything, including activities you once enjoyed |
| Sleep Issues | Trouble falling asleep (“wired but tired”); racing thoughts about work | Early morning waking (3-5 AM); or sleeping excessively but still exhausted |
| Concentration | Brain fog during work tasks; forgetfulness related to stress | Difficulty concentrating on everything; indecisiveness across all areas |
| Physical Symptoms | Tension headaches, tight shoulders, digestive issues (stress-related) | Unexplained body aches, changes in appetite, psychomotor changes |
| Triggers | Identifiable stressor (demanding job, caregiving, chronic overwork) | No clear external cause; can be endogenous (internal neurobiological) |
| Recovery Pattern | Improves with time off, boundaries, job change | Doesn’t improve with situational changes alone; needs treatment |
| Self-Perception | “I’m exhausted by my work” | “I’m worthless” or “Nothing matters” |
| Timeline | Often tied to a specific period of high stress | Can persist for months or years without intervention |
Key Insight: Symptoms Overlap, But Biology Doesn’t
Notice how much overlap there is? That’s why questionnaires fail. But here’s what matters: even though the symptoms look similar, the underlying biology is different.
- Burnout = Your stress response system (HPA axis) is dysregulated from chronic overwork
- Depression = Your neurotransmitter systems (serotonin, dopamine, norepinephrine) are disrupted
That’s why antidepressants might not work if you’re burned out. And why “just take a vacation” won’t fix clinical depression.
So how do you know which one you have? That’s where lab testing comes in.
5 Tests That Might Differentiate Between Burnout and Depression
You know the symptoms overlap. Questionnaires aren’t enough. So what actually helps?
Your body’s data. No single lab will hand you a diagnosis, but specific tests can show whether you’re dealing with a stress response that’s gone haywire or something deeper happening with your brain chemistry.
Important: These tests aren’t about getting a label—they’re about understanding what’s actually broken so you can fix the right thing.
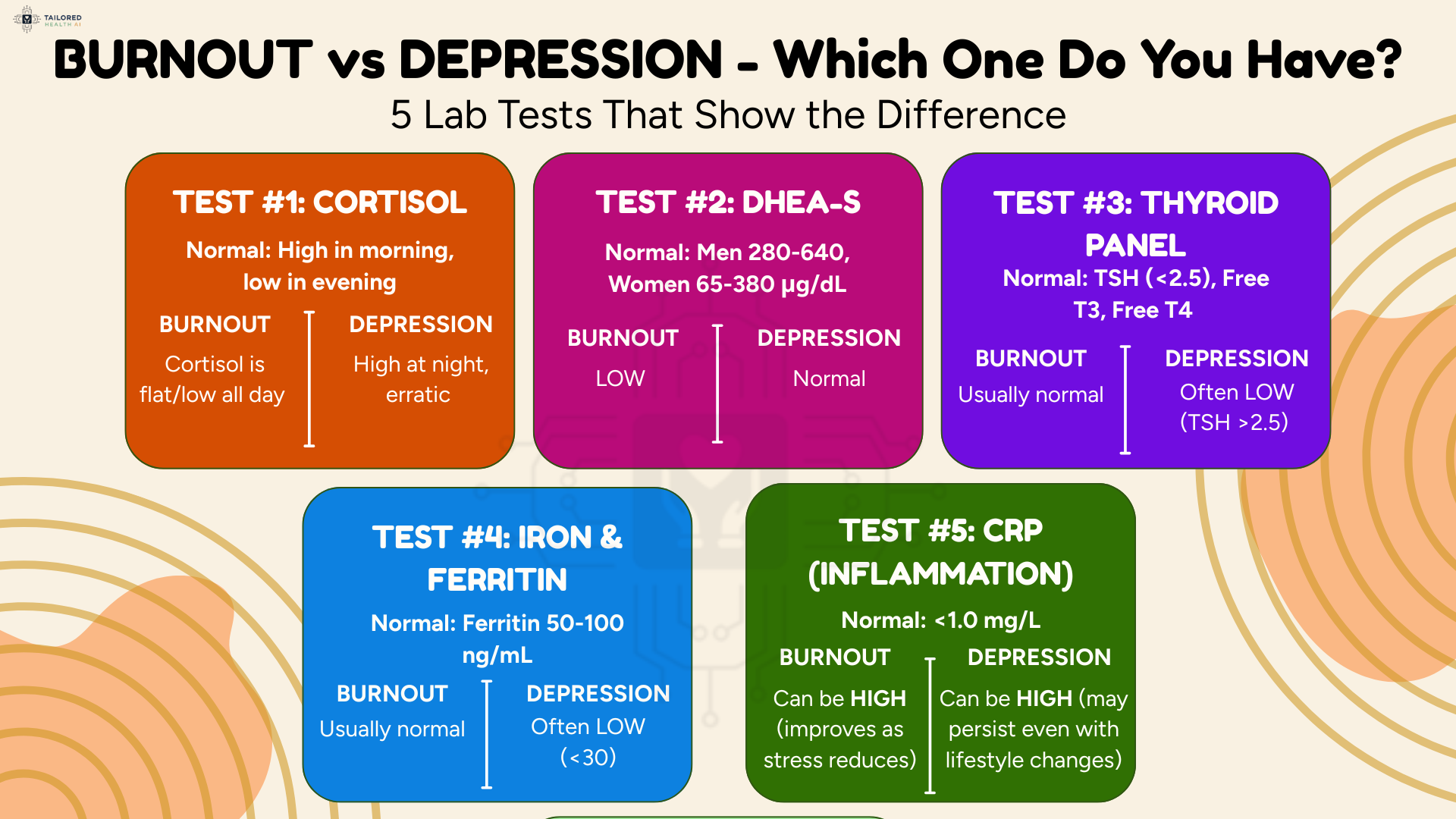
Test 1: 4-Point Cortisol Test
This test measures your cortisol levels at 4 different times throughout the day (morning, noon, evening, and bedtime). Cortisol is your primary stress hormone, and it should follow a natural rhythm—high in the morning to help you wake up, then gradually declining throughout the day (Cleveland Clinic).
What the patterns look like:
If you have burnout:
- In early stages, your cortisol may be elevated throughout the day, especially in the morning and evening. This is the “wired but tired” feeling—you’re exhausted but can’t relax
- In advanced burnout, your cortisol curve flattens completely. Your stress response system is so exhausted that cortisol stays low all day
If you have depression:
- Your morning cortisol awakening response may be disrupted (cortisol doesn’t rise properly when you wake up).
- The rhythm is irregular, but the underlying mechanism is different from burnout and not necessarily tied to an identifiable stressor.
Why this matters:
If your cortisol is dysregulated—either sky-high or completely flatlined—antidepressants alone won’t fix it. You need interventions that address your stress response system (like adaptogens, nervous system regulation, and setting boundaries).
Test 2: DHEA-S Test
This test measures DHEA-S, a hormone produced by your adrenal glands that acts as a counterbalance to cortisol. It supports resilience, mood, and energy. When you’re under chronic stress, DHEA levels often drop while cortisol stays elevated or dysregulated (NIH).
What the patterns look like:
If you have burnout:
- Your DHEA-S levels are often low, indicating that your adrenal reserves are depleted.
- The DHEA-S to cortisol ratio is low, which signals high stress and low resilience. This pattern is a strong indicator that your stress response system is exhausted.
If you have depression:
- DHEA levels may also be lower, but the ratio and context are different.
- The pattern isn’t necessarily tied to a specific chronic stressor like work or caregiving.
Why this matters:
The DHEA-S to cortisol ratio is one of the most reliable biomarkers for chronic stress and burnout. If your DHEA is tanked, you need interventions that support adrenal function—not just antidepressants.
Stop Guessing. Get Personalized Answers.
✅ Symptoms (burnout, depression, thyroid issues, or deficiencies)
✅ Lab results (cortisol, inflammation, thyroid, nutrient levels)
✅ Lifestyle factors (stress, sleep, diet, work patterns)
Then creates your personalized health optimization plan
🎉 First 100 Founding Members Get 50% OFF
Test 3: Inflammatory Markers (CRP, ESR)
This test measures CRP (C-Reactive Protein) and ESR (Erythrocyte Sedimentation Rate), which are general markers of inflammation in your body.
Here’s the catch: both burnout and depression are associated with elevated inflammation, so this test alone won’t differentiate between them. But it adds important context.
What the patterns look like:
If you have burnout:
- Your CRP is often elevated because chronic stress triggers inflammatory pathways in your body.
- This inflammation is often paired with cortisol dysregulation or adrenal dysfunction.
- The good news: inflammation may improve relatively quickly once you start addressing stress.
If you have depression:
- Your CRP may also be elevated due to neuroinflammation, which is linked to depression.
- The inflammation may persist even with lifestyle changes and often requires anti-inflammatory interventions in addition to other treatments.
Why this matters:
If your inflammation is high, it’s contributing to your fatigue and brain fog—regardless of whether you have burnout or depression. Addressing inflammation through a balanced diet, omega-3 fatty acids, and maintaining gut health should be part of your recovery plan.
Test 4: Full Thyroid Panel
This test measures TSH (Thyroid Stimulating Hormone), Free T3, Free T4, and thyroid antibodies.
Why include thyroid? Because hypothyroidism can mimic both burnout and depression (Activated Health & Wellness). The symptoms: fatigue, brain fog, low motivation, weight changes look almost identical.
What to look for:
- High TSH combined with low Free T3 and Free T4 indicates hypothyroidism. This needs to be treated first before addressing anything else.
- Normal TSH but low Free T3 can indicate poor thyroid hormone conversion, which is common when you’re under chronic stress. (NIH)
- The presence of thyroid antibodies indicates autoimmune thyroid disease (Hashimoto’s), which requires a different treatment approach.
Why this matters:
If your thyroid function is off, no amount of stress management or antidepressants will fully resolve your symptoms until you address the thyroid issue. Chronic stress can suppress thyroid function, and low thyroid can worsen or even cause depression
Free Download: Good Mood Toolkit
Test 5: Nutrient Deficiency Panel
This test measures key nutrients that directly impact your energy, mood, and brain function: Vitamin D, B12, Iron/Ferritin, and Magnesium.
Deficiencies in any of these nutrients can mimic or worsen both burnout and depression.
What each nutrient does:
- Vitamin D: Low levels are strongly linked to depression, fatigue, and immune dysfunction (Healthline). It’s especially common in people who work indoors or live in northern climates.
- Vitamin B12: This is essential for energy production and nervous system function. Deficiency causes fatigue, brain fog, and mood issues (Graphic Era Hospital). It’s common in vegetarians/vegans, people with gut issues, and older adults.
- Iron/Ferritin: Low iron means your tissues aren’t getting enough oxygen, which causes exhaustion (Mayo Clinic). Ferritin (stored iron) can be “normal” on labs but still suboptimal. Women with heavy periods are especially at risk.
- Magnesium: This mineral is involved in over 300 biochemical reactions in your body, including stress response (NIH). It gets depleted by chronic stress. Deficiency causes anxiety, insomnia, and muscle tension.
Why this matters:
If you’re deficient in any of these nutrients, you’ll feel exhausted and depressed no matter what else you do. These are foundational—fix them first before pursuing other treatments.
Ready to Figure Out What’s Actually Wrong?
Tailored Health AI gives you:
✅ Clear pattern identification (burnout, depression, thyroid, nutrient deficiencies, or combination)
✅ Personalized supplement recommendations based on YOUR labs
✅ Lifestyle protocols tailored to YOUR stressors
✅ Guidance on when to seek professional help
🎉 First 100 Founding Members: 50% OFF
FAQs: Your Common Questions Answered Here
⚠️Important Information
This article is for educational purposes only and is not medical advice. Always consult with a qualified healthcare provider before making decisions about your health, diagnosis, or treatment.

