What Is Male Infertility? Understanding Causes and Treatment
Introduction
What Is Male Infertility? Definition
Male infertility is a medical condition where a man has difficulty contributing to conception despite regular, unprotected sexual intercourse for at least 12 months. Simply put, it means a man’s reproductive system isn’t working optimally to help create a pregnancy.
What Does Male Infertility Mean in Simple Terms?
It’s important to understand that male infertility doesn’t mean a man is completely sterile or can never father children. Men’s infertility indicates there are challenges with one or more of these key areas:
- Sperm production (The body creates too few sperm, resulting in a low sperm count)
- Sperm function (problems with sperm motility: sperm that swim weakly or in the wrong direction)
- Sperm delivery (getting sperm where it needs to go)
Men’s fertility challenges vary in severity, and most men with fertility problems can be successfully treated with appropriate medical intervention. In this article, we will understand male infertility by understanding the normal sperm morphology, normal sperm count, and percentage of infertility in men, followed by causes, symptoms, prevention, and treatment of male infertility.
Understanding Normal Sperm Parameters
Healthy sperm are essential for natural conception. Sperm quality depends on three main factors that doctors evaluate during fertility testing.
1. What Is the Normal Sperm Count in Males?
Normal sperm count falls between 15 million and 200+ million sperm in each milliliter of ejaculation.
| Sperm Count Category | Sperm per Milliliter | Fertility Impact |
|---|---|---|
| Normal | 15+ million | Good fertility potential |
| Low (Oligospermia) | Below 15 million | May affect conception |
| Very Low | Below 5 million | Significant fertility challenges |
The average adult male produces around 100-300 million sperm cells daily, with some sources citing approximately 170 million sperm daily.
2. What Is Normal Sperm Motility?
Normal sperm motility means that at least 40% of sperm can swim forward effectively:
- Progressive motility: Forward-swimming sperm (minimum 32% needed for normal fertility)
- Non-progressive motility: Sperm moving but not forward, or those moving in tight circles.
- Immotile: Sperm that don’t move at all.
Non-progressive motility and immotile sperm compromise sperm health because sperm must move efficiently through reproductive pathways to achieve fertilization.
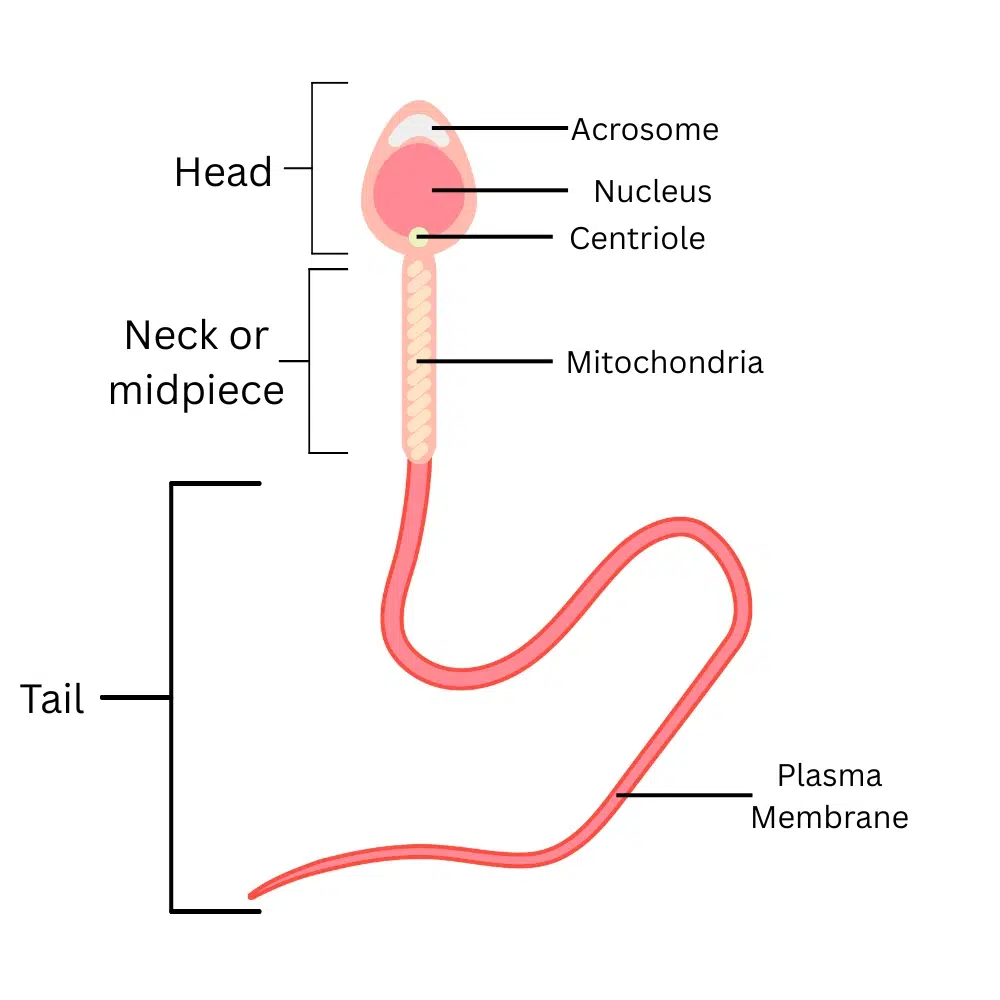
3. Normal Sperm Morphology: What Should Sperm Look Like?
Healthy sperm require proper structure to function effectively:
- Head: Oval-shaped with smooth contours
- Neck and midpiece: Well-defined connection
- Tail: Long, straight, and uncoiled
Just 4% of sperm should be of an ideal morphology to fertilize an egg. This low percentage works because sperm production generates millions so providing adequate healthy sperm for fertilization.
How Is Sperm Produced? The Sperm Creation Process
Sperm production occurs within the testicles via spermatogenesis. This video shows how healthy sperm are made:
Video Credits: Julia Lerner
The 74-Day Journey:
- Stem cells in the testicles start dividing
- Immature sperm cells develop over 64 days inside tiny tubes
- Maturing sperm cells move into the epididymis, where they complete their 10-day development process.
- Mature and healthy sperm are stored until ejaculation.
How Common Is Male Infertility? Understanding the Statistics
Male fertility issues are more widespread than many people realize, affecting millions of men worldwide.
Research shows that:
- 7-12% of men experience fertility challenges at some point (NCBI)
- It affects approximately 1 in 6 men globally (WHO)
- Male infertility affects an estimated 15% of couples globally, with males being solely responsible for 20-30% of infertility cases and contributing to 50% of cases overall. (NCBI)
Male Infertility Rates by Country
| Country/Region | Male Infertility Rate |
|---|---|
| USA (North America) | 4.5-6% |
| Canada (North America) | 4.5-6% |
| UK (Europe) | 7.5% |
| Australia | 8% |
Male Fertility and Age: When Are Men Most Fertile?
Understanding the relationship between male fertility and age is crucial for couples planning to start a family. While men can produce sperm throughout their lives, fertility quality and quantity change significantly with age.
Research indicates that peak male fertility occurs around ages 25-30, with sperm quality declining after age 30. (NCBI)
What Causes Male Infertility?
Male infertility causes can be complex, but understanding them helps identify potential solutions. These causes fall into several main categories that affect sperm production, function, or delivery.
Sperm Production Problems
- Varicocele: Swollen blood vessels within the scrotum that disrupt normal sperm development and function
- Hormonal Imbalances: Insufficient production of key reproductive hormones like FSH, LH, and testosterone that are essential for sperm creation. Estrogen dominance in men can also disrupt this hormonal balance, suppressing sperm production and reducing fertility. High estrogen levels relative to testosterone interfere with the body’s natural reproductive processes.
- Genetic Conditions: Inherited disorders, such as Klinefelter syndrome, that impair the body’s ability to produce healthy sperm
- Infections: Various infections that damage sperm-producing cells or affect sperm function:
- Sexually transmitted infections (chlamydia, gonorrhea, syphilis)
- Mumps (when occurring after puberty)
- Prostatitis and urinary tract infections (UTI)
What Causes a Man Not to Produce Sperm?
Complete absence of sperm (azoospermia) has specific causes:
- Genetic Disorders: Conditions that completely prevent sperm production (Klinefelter Syndrome (XXY), Y Chromosome Microdeletions, Kallmann Syndrome, Noonan Syndrome)
- Severe Infections: Infections that permanently damage sperm-producing cells (Mumps Orchitis, Severe Epididymitis, Tuberculosis (TB) of the Reproductive Tract, Severe Prostatitis, Post-Surgical Complications)
- Cancer Treatments: Chemotherapy and radiation that destroy sperm-producing tissue
- Severe Hormonal Deficiencies: Complete lack of hormones needed for sperm production
- Congenital Absence of Vas Deferens (CAVD): Born without the tubes that carry sperm
The key difference is that genetic disorders typically affect sperm production at the cellular level, while severe infections usually cause physical blockages or destroy the tissue that produces or transports sperm.
What Causes Weak or Dead Sperm? Sperm Function Problems
Poor sperm motility results from:
- Infections: Bacterial or viral infections that weaken sperm or reduce their ability to move
- Antioxidant Deficiencies: Lack of protective nutrients leading to sperm damage
- Age-Related Decline: Natural reduction in sperm quality as men get older
Physical and Functional Problems
- Erectile Dysfunction: Difficulty maintaining an erection long enough to achieve conception.
- Premature Ejaculation: Challenges in attaining or maintaining an erection adequate for sexual activity.
- Retrograde Ejaculation: A medical condition where, during the climax, semen is redirected into the bladder rather than being ejaculated out through the penis.
- Hernias: Abdominal wall defects that may compromise blood circulation to the reproductive organs
Lifestyle and Environmental Causes
- Lifestyle Factors
- Heat Exposure: Hot tubs, saunas, laptops on lap, tight clothing
- Smoking and Excessive Alcohol: Toxic substances that deteriorate sperm health and interfere with normal production processes
- Stress and Poor Diet: Can disrupt hormone balance and sperm quality
- Obesity and Lack of Exercise: Excess weight and a sedentary lifestyle disturb hormonal balance and impair fertility
- Medications and Substances
- Anabolic Steroids: Shut down natural hormone production
- Prescription Medications: Certain antidepressants, blood pressure medications, and others
- Recreational Drugs: Can temporarily or permanently affect sperm production
- Environmental Toxins
- Heavy Metal Exposure: Contact with toxic elements like lead and mercury that damage reproductive cells
- Pesticides and Chemicals: Exposure to agricultural toxins and industrial compounds that harm male fertility
- Radiation Exposure: From medical treatments or occupational hazards
- Workplace Heat: Jobs involving high temperatures or prolonged sitting
Male infertility rarely has a single cause. Often, multiple factors combine to create fertility challenges.
Get Your Personalized Male Fertility Assessment
recommendations.
Signs and Symptoms of Male Infertility
The Main Indicator of Male Infertility
Failure to achieve pregnancy after 12 months of consistent, unprotected sexual activity serves as the main indicator of male fertility issues. This is often the only symptom that alerts couples to seek medical evaluation.
Male Infertility Symptoms
Important Note: These signs and symptoms do not definitively indicate male infertility. Instead, they may point to underlying conditions such as hormonal imbalances, infections, or other medical issues that could potentially affect fertility. Many men with these symptoms have normal fertility, while others with no symptoms at all may have fertility problems.
- No pregnancy achieved following 12 consecutive months of regular sexual activity without contraception
- Difficulty with erections or maintaining them during intercourse
- Ejaculatory difficulties, including premature release, delayed climax, or discomfort during orgasm
- Reduced sexual desire or low libido
- Testicles that are unusually small in size or have an abnormally hard texture
- Discomfort, aching, or enlargement in the testicular area or scrotal sac
- Visible enlarged veins in the scrotum (varicocele)
- Very low ejaculate volume or watery semen
- Blood in semen or unusual semen color/smell
- Reduced facial or body hair growth
- Breast enlargement (gynecomastia)
- Unexplained fatigue and low energy
- Decreased muscle tissue or challenges in developing muscular strength
- Weight gain around the midsection
- Recurrent genital infections or unusual discharge
- History of undescended testicles or testicular injury
- Chronic respiratory infections (may indicate genetic conditions)
What are the Fertility Tests for Men?
Fertility testing for men can provide essential insights, guiding you toward informed next steps with confidence and care. This guide delivers the essentials: when to test, what’s involved, and why it matters—all in a professional, easy-to-read format.
- When to Test: Know the Signs
- Timing: Consider testing after 6-12 months of unsuccessful attempts to conceive.
- Risk Factors: Men over 40, or those with a history of testicular issues, cancer treatments, or toxin exposure, should test sooner.
- Partner Approach: Testing alongside your partner often yields the best insights.
Semen Analysis: The Starting Point
Semen analysis is the essential first step in evaluating male fertility, offering critical insights into reproductive health with care and precision (WHO)
- Preparation for Testing: To achieve reliable results, avoid ejaculation for 2-5 days before the test. The sample should be collected in a sterile container provided by the clinic and transported to the lab, ideally within an hour, to maintain accuracy
- Key Metrics:
- Sperm Count: At least 15 million sperm per milliliter or 39 million total per ejaculate to support fertility.
- Sperm Motility: 40% or more of sperm should exhibit strong, forward movement to reach the egg.
- Sperm Morphology: 4% or more of sperm should have a normal shape to penetrate the egg effectively.
- Semen Quality: Semen volume of 1.5-5 mL, pH of 7.2-8.0, and minimal white blood cells to ensure a supportive environment for sperm.
- Follow-Up Testing: Sperm test results can fluctuate due to factors like stress or illness, so repeat testing may be necessary to confirm findings and ensure a precise diagnosis.

What Blood Tests are done for Male Infertility?
Testing these hormones can uncover underlying issues that may quietly impact fertility, providing a path to targeted solutions.
- Testosterone: Drives sperm production.
- FSH & LH Evaluation: These hormones play a vital role in regulating sperm production and maintaining hormonal balance, guiding the body’s reproductive processes.
- Prolactin: Excess prolactin can lead to problems like low sex drive, difficulty in maintaining an erection, and premature ejaculation.
Physical Examination
A physician will perform a thorough assessment of key reproductive structures to identify any abnormalities:
- Testicles: The doctor will evaluate testicular size, consistency, and the presence of any masses or swelling to confirm optimal function for sperm production.
- Varicoceles: Enlarged veins in the scrotum, which may elevate testicular temperature and impair sperm quality, will be carefully examined, as they are a treatable cause of infertility.
- Penis and Urethra: A brief inspection ensures no structural abnormalities, such as atypical urethral openings, that could hinder sperm ejaculation.
- Prostate and Epididymis: These structures, critical for sperm storage and semen production, are assessed for signs of blockages, inflammation, or infection.
Advanced Diagnostic Tests
For complex cases, specialized diagnostics can be recommended to pinpoint underlying causes:
- Genetic Testing: When semen analysis reveals very low or absent sperm, blood tests can identify chromosomal or genetic factors contributing to infertility.
- Testicular Biopsy: If no sperm is detected in semen, a minor procedure to collect a testicular tissue sample can determine whether the issue stems from a blockage or impaired sperm production.
- Anti-Sperm Antibody Testing: This test investigates whether the immune system is producing antibodies that attack sperm, leading to clumping and reduced fertility.
- Ultrasound Imaging: Scrotal or reproductive tract imaging can detect blockages, structural anomalies, or other irregularities impacting fertility.
At-Home Kits: A First Glance
At-home fertility tests, like SpermCheck or Trak, offer a quick, private way to check sperm count in 10-20 minutes. You collect a sample and follow simple instructions to get basic results at home. These kits are great for an initial look, especially if visiting a clinic feels daunting.
Limitations of At-Home Tests:
While at-home kits offer a convenient starting point for assessing sperm count, they cannot evaluate crucial aspects such as sperm motility, shape, or the quality of seminal fluid, necessitating professional testing for a comprehensive diagnosis.
Skip the Guesswork. Get Your Custom Fertility Plan
What Should a Man Eat To Boost Fertility?
A fertility diet plan for men can improve sperm count, quality, and motility by up to 70% within three months. Since sperm takes 74 days to develop, the foods you eat today directly impact your fertility potential.
The diet to increase fertility in men focuses on nutrient-dense foods that support sperm production while avoiding harmful substances that damage reproductive health.
Top Fertility Foods for Men
1. Sunflower Seeds – The Fertility Powerhouse
Sunflower seeds increase sperm count more effectively than many expensive supplements. These tiny seeds pack incredible fertility benefits:
- Vitamin E: Protects sperm from damage
- Selenium: Boosts sperm formation by 52%
- Zinc: Essential for testosterone production
- Folate: Prevents genetic abnormalities

How to use: Add 1 ounce (handful) daily to smoothies, salads, or snacks. Regular consumption of sunflower seeds significantly increases sperm volume.
2. Antioxidant-Rich Fruits
Food for healthy sperm must include powerful antioxidants:
- Berries: Blueberries and strawberries improve sperm motility by 23%
- Pomegranates: Rich in vitamin C and folate
- Citrus fruits: Support sperm DNA health
- Dark grapes: Contain resveratrol for better sperm quality
Berries

Pomegranate

Citrus Fruits

Black Grapes

3. Leafy Green Vegetables
Essential foods to increase male fertility:
- Spinach: Spinach is high in folate, an essential vitamin for sperm production
- Kale: Rich in antioxidants and iron
- Broccoli: Contains vitamin C and folate
- Asparagus: Natural source of vitamin E
Spinach

Kale

Broccoli

Aspasragus

4. Healthy Protein Sources
Quality proteins that support hormone production:
- Wild salmon: Wild salmon contains Omega 3, an essential fatty acid for sperm function and production.
- Lean chicken: Complete protein for muscle and hormone support
- Eggs: Choline for sperm membrane health
- Lentils: Plant-based protein with folate
Wild Salmon

Lean Chicken

Eggs

Lentils

5. Nuts and Healthy Fats
- Walnuts: Improve sperm shape and movement
- Almonds: Vitamin E for antioxidant protection
- Avocados: Healthy monounsaturated fats
- Olive oil: Reduces inflammation
Walnuts

Almonds

Avocados

Olive Oil

Which Food Reduces Sperm?
Foods that reduce sperm quality and should be limited:
- Processed meats: Bacon, sausages, and deli meats can decrease sperm concentration
- Trans fats: Margarine, commercial baked goods, and deep-fried foods damage sperm quality
- Excessive soy: Large amounts may interfere with testosterone production
- High-mercury fish: Shark, king mackerel, certain tuna varieties, and kingfish that have high mercury, as these can affect fertility.
- Sugary beverages: Sugary drinks can lead to an increase in oxidative stress, which can hamper proper sperm production.
- Refined carbohydrates: White flour products and processed snacks spike blood sugar
What are the Best Male Fertility Supplements?
When trying to conceive, choosing the right fertility supplements for men can significantly improve sperm quality and count. Here are what vitamins a man should take when trying to conceive, backed by research and proven results.
Male Fertility Vitamins
| Vitamins | Function |
|---|---|
| Vitamin C (500-1000mg daily) | Studies show vitamin C supplements may help improve semen quality and partner pregnancy rate. This powerful antioxidant protects sperm from damage while supporting healthy development. |
| Vitamin E (400 IU daily) | Take with selenium for maximum benefits. Vitamin E acts as a protective shield for sperm membranes and improves overall sperm function when combined with other antioxidants. |
| Vitamin B12 (2.4mcg daily) | Clinical studies reveal that B12 supplementation enhances sperm production and maintains healthy DNA integrity. B12 supports the metabolic processes required for healthy sperm cell development. |
| Folic Acid (5mg daily) | Research indicates that folate works synergistically with zinc to boost sperm count. Folate aids in the genetic material formation process within developing sperm. |
| Vitamin D (1000-2000 IU daily) | Men with adequate vitamin D levels show improved testosterone production and better sperm quality. Vitamin D helps optimize the mineral balance necessary for optimal sperm movement. |
Critical Minerals for Male Fertility
| Minerals | Function |
|---|---|
| Zinc (15-30mg daily) | Clinical trials demonstrate that zinc supplementation significantly increases semen volume and improves sperm movement patterns. This mineral is concentrated in male reproductive tissues and supports testosterone synthesis. |
| Selenium (100-300mcg daily) | Long-term selenium supplementation over several months enhances sperm swimming ability and improves sperm shape quality. This trace mineral functions as a powerful antioxidant in reproductive tissues. |
| Iron (8mg daily) | Adequate iron levels support oxygen transport to reproductive organs and maintain healthy sperm production. Low iron also affects sperm count and motility leading to low sperm count and slow-swimming sperm. |
| Magnesium (400mg daily) | This mineral supports enzyme functions involved in sperm development and maintains cellular integrity in reproductive tissues. Magnesium additionally aids in the production of testosterone. |
Best Fertility Supplements for Men
| Supplement | Function |
|---|---|
| Coenzyme Q10 (200-300mg daily) | Research shows that CoQ10 levels in seminal fluid correlate directly with sperm quality parameters. This enzyme provides cellular energy needed for sperm movement and function. |
| D-Aspartic Acid (2.66g daily) | Clinical studies demonstrate that D-AA supplementation can increase testosterone levels and dramatically improve sperm count within three months. This amino acid stimulates hormone production naturally. |
| L-Arginine (1-3g daily) | L-arginine enhances circulation to male reproductive tissues and organs. It also helps maintain proper sperm membrane function. |
| Omega-3 Fatty Acids (1-2g daily) | Essential fatty acids improve sperm membrane fluidity and support healthy sperm development. Omega-3s are vital components for maintaining sperm cell integrity and performance. |
| N-Acetyl Cysteine (600mg daily) | NAC provides protective benefits against cellular damage while promoting optimal sperm genetic health. NAC also supports ideal sperm density. |
| L-Carnitine (2-3g daily) | L-carnitine enhances sperm energy production and significantly improves sperm concentration, motility, and overall quality. Clinical studies show marked improvements in fertilization rates. |
Vitamins to Increase Sperm Volume
Zinc remains the primary nutrient for men looking to increase seminal fluid volume. Zinc accumulates in the prostate and seminal vesicles, where it aids seminal fluid formation. L-arginine (1-3g daily) supports healthy blood flow to reproductive organs.
Male Fertility Tips for Success
- Timing Matters: Since sperm development takes 74 days, the best fertility vitamins for men require consistent use for at least 3 months to see results.
- Combination Approach: A multi-nutrient strategy combining D-Aspartic Acid, CoQ10, Zinc, Folic Acid, and Vitamin E delivers enhanced reproductive outcomes. Comprehensive male fertility pills often work better than single nutrients.
- Quality Selection: Choose men’s fertility vitamins from reputable manufacturers with third-party testing. Choose easily absorbed formulations without excess fillers or artificial ingredients.
Get Your Tailored Supplement Protocol
How is Male Infertility Treated?
When it comes to male infertility treatment, modern medicine offers proven solutions that can restore your fertility and help you achieve your family goals. The key is identifying the right medical approach based on your specific condition.
Fertility Drugs for Men
Fertility drugs for men have revolutionized treatment outcomes. These aren’t experimental treatments – they’re FDA-approved medications with solid success rates:
| Medication | What It Treats | How It Works | Success Rate |
|---|---|---|---|
| Clomiphene Citrate (Clomid) | Low testosterone, and poor sperm production | Stimulates brain to release testosterone that boost sperm production | 60-70% improvement in sperm count. |
| Human Chorionic Gonadotropin (hCG) | Hormonal imbalances and undescended testicles | Directly stimulate testosterone and sperm production | 40-60% pregnancy rate. |
| Follicle Stimulating Hormone (FSH) | Very low sperm count, hormonal deficiencies | Directly targets sperm-producing cells in testicles | 30-50% improvement in sperm parameters. |
| Anastrozole (Arimidex) | High estrogen levels affecting fertility (estrogen dominance) | Blocks estrogen production, restores hormonal balance | 65-80% improvement in testosterone levels. |
Advanced Medical Procedures
When male infertility medicine alone isn’t sufficient, advanced procedures step in:
| Procedure | Best For | Success Rate | Recovery Time |
|---|---|---|---|
| Varicocele Repair | Enlarged scrotal veins affecting sperm | 60-80% improvement | 2-3 weeks. |
| Sperm Retrieval (TESE/MESA) | No sperm in ejaculate | 50-70% sperm retrieval rate | 1-2 weeks. |
| Vasectomy Reversal | Previous vasectomy | 85-95% sperm return rate | 4-6 weeks. |
| Intracytoplasmic Sperm Injection (ICSI) with IVF | Severe male factor infertility | 60-70% pregnancy rate | Outpatient procedure. |
IVF Treatment for Male Infertility
When natural conception isn’t possible, IVF treatment for male infertility offers the highest success rates. ICSI (Intracytoplasmic Sperm Injection) can work even with severely compromised sperm, requiring just one healthy sperm per egg.
The process involves retrieving eggs from your partner, selecting the best available sperm (even if numbers are extremely low), and directly injecting sperm into eggs in the laboratory. Pregnancy rates typically fall between 60% to 70% per attempt, with outcomes influenced by the couple’s age and medical conditions.
Treatment for male infertility typically produces measurable improvements in 3-6 months, since the complete sperm production cycle requires approximately 10-11 weeks.
When to Seek Medical Help for Male Infertility
If you’re concerned about male infertility, taking action early can make a big difference. Knowing when to seek medical help and which specialist to consult is the first step toward better reproductive health. Here’s what to look for and the types of doctors who can assist.
Signs/Symptoms That Indicate It’s Time to See a Specialist
Certain signs suggest it’s time to visit a male fertility doctor near me. If you observe any of these signs, it’s wise to consult a specialist promptly:
- Difficulty achieving or maintaining an erection, which could signal underlying fertility issues.
- Discomfort, inflammation, or a noticeable mass in the testicles, which could impact sperm production.
- Low sex drive or hormonal imbalances that impact male fertility.
- A past testicular injury or surgical procedure, that potentially needs expert assessment.
- No pregnancy after a year of regular, unprotected sex with your partner (or six months if over 35).
What kind of Doctor specializes in Male Infertility?
Gaining insight into the various doctors who address male infertility can guide you toward the best specialist for your needs. Here are the main options:
- Urologist: A urologist specializes in the male reproductive and urinary systems, offering expertise in related health concerns. They can treat infertility issues like blockages or varicose veins in the scrotum.
- Andrologist: An andrologist focuses on male-specific health, emphasizing fertility and hormonal balance. They are skilled at diagnosing and addressing conditions such as reduced sperm count or testosterone imbalances.
- Reproductive Endocrinologist: This doctor specializes in hormones and fertility for both men and women. They often step in for complex cases, such as severe hormonal imbalances affecting male fertility.
Each specialist brings unique skills, so discussing your symptoms with a male fertility doctor near me can help determine the best fit for your needs.

